Type 2 Diabetes mellitus (NIDDM) , is a cluster of factors coming together to cause hyperglycemia. The two predominant factors are insulin resistance and declining beta cell function. Either factor on its own may not manifest with type 2 diabetes, but together pose a lethal threat for the pancreas resulting in pancreatic decline and consequent hyperglycemia.
Insulin resistance is required a physiological change that occurs in the healthy individual during certain phases of life.
- Puberty is the first such change. There is diversion of energy from utilization by the muscle to growing cells to promote vertical growth and increased muscle mass. This is probably due to the effect of Growth hormone and cortisol
- Pregnancy. The foetus secretes hormones into maternal circulation that induces insulin resistance This prevents the liver from converting glucose to glycogen and diverts this to the placenta. The mother secretes increased amounts of insulin. When the maternal pancreatic output is overwhelmed, this can result in gestational diabetes.
- Infection. Several factors promote insulin resistance during illness. Oral consumption may be minimal, but the body requires energy for the battle. It secretes stress hormones which induces insulin resistance and prevention of storage of glucose. Energy is required for immune cells, repair and survival
Insulin resistant and metabolic syndrome
Insulin resistance is perhaps the main factor that starts the process off towards diabetes. While there are undoubtedly genetic factors for insulin resistance, environmental factors also play a role. As we transition from teenagers ( when we are very active, ) and settle into work as young adults, our food habits, activity levels are all adversely affected. Food becomes more available and more calorie dense. . With declining activity , increased insulin secretion is required and this promotes the storage of glucose ( rather than utilization). As our muscles and liver fill up with glycogen ( which is not utilized, insulin promotes the conversion of glucose into trigylcerides. As our fat storage starts filling up, higher levels of insulin is required for glucose disposal. This vicious cycle of increasing insulin requirement is called insulin resistance. probably existed for several years before Type 2 diabetes manifests. A combination of reduced exercise, ( reduced utilization of glucose) and increased consumption of carbohydrates results in increasing demand on the pancreas to put out insulin to store glucose.
While insulin resistance for a short duration, is essential, in the long term the pancreas may struggle with the increasing demands. The robust plasticity of the pancreas is overwhelmed.
Early changes – still normoglycemia
The first change that occurs is loss of the first phase of insulin secretion. Insulin is normally produced and stored in the beta cell for rapid release when food is ingested. This is called the first phase of insulin secretion. This rapid release of stored insulin from beta cells ensures rapid capture of passing glucose by the hepatocytes and normoglycemia in the peripheral tissue.
With insulin resistance, there is constant hypersecretion of insulin and a decline in amount of stored insulin. The first phase of insulin secretion declines and there is mild peripheral rise in glucose.
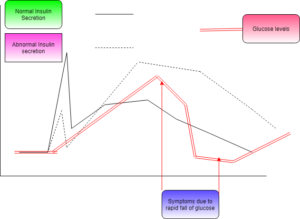
The above picture is the response of pancreatic islets to a meal. The first figure shows normal pancreatic islet secretion. The second is from a person with insulin resistance and impaired glucose tolerance
The only measurable values are raised levels of post-prandial glucose ( although still in the normal range)
Further progression – impaired glucose tolerance
This is manifest by rising levels of fasting insulin. This indicates progression of insulin resistance and constant insulin hypersecretion. Higher levels of insulin is required to maintain normoglycemia in the fasting state. There is also fasting hypertriglyceridemia. the period of post prandial rise in glucose takes longer to come into normal range
Pancreatic damage – Early Type 2 diabetes
In the pancreas, beta cells in the islets start falling. There is amyloidosis around the islets. This may be due to misfolded proteins secreted from the islets. Fasting blood sugars start rising and fall into the impaired fasting glucose range. There is significant fasting and post-prandial hyper insulinemia. lipid profile starts getting affected with hyper triglyceridemia, low HDL lipoprotein ( Diabetic dyslipidemia). This phase is reversible and significant loss of body weight or increase in energy expenditure , can put diabetes in remission.
Progressive Pancreatic damage – established type 2 diabetes
With established Type 2 diabetes, the person may still be completely asymptomatic due to the insidious nature of progression. There is rising fasting blood glucose levels with significant post prandial glucose excursions. There is significant hyper insulinemia at all times. The pancreatic beta cells decline in number with increasing amyloidosis around the islets. ( this may be due to deposition of misfolded proteins secreted from the islet.
The following differences are observed..
- Fasting insulin levels are higher
- The insulin levels are higher levels
- The duration of insulin secretion is longer.
- There is longer period of hyperglycemia